H. Pylori Natural Treatment Guide: Symptoms, Diet, Herbals
H. pylori was the first bacteria to be formally recognized as a carcinogen and is an underlying root cause of many gastrointestinal disorders. Researchers and sufferers have been wanting to find how to cure H. pylori since its role in stomach ulcers was discovered over 30 years ago. And with the conventional triple antibiotic therapy no longer considered the best or only choice, H. pylori natural treatment approaches have become increasingly well researched, effective and preferred in clinical practice in recent years.
Having helped hundreds of clients at The Functional Gut Health Clinic eradicate H. pylori in recent years using natural protocols, we’re excited to share both our understanding and current approach.
[Last Updated: May 2024]
Here’s everything we’re going to cover:
What is Helicobacter pylori (H. pylori)
How do you catch it and how prevalent is H. pylori?
What diseases can it cause?
Symptoms of H. pylori
H. pylori testing options available
H. pylori natural treatment protocols we use
Using Matula Tea for H. pylori and other natural options
Access to our Fullscript Dispensary and 20% Off H. pylori supplements
What is Helicobacter pylori?
Helicobacter pylori (H. pylori) is a gram-negative bacteria that has a helical rod-shaped body with sheathed flagellae, which look like tails. The flagellae move to propel H. pylori around the body. It is a gram-negative bacteria, which means it has a double cell membrane, making it more resistant to interventions. Although it has been co-evolving with humans for 58,000 years, it was only discovered by two Australian researchers in 1982, who went on to win the Nobel Prize for their discovery in 2005.
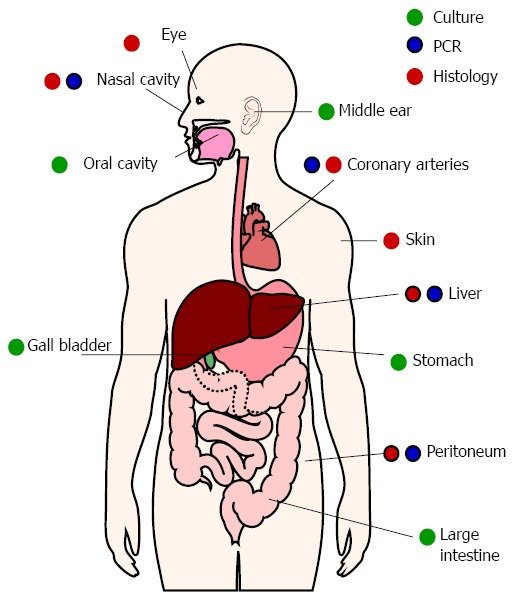
We often focus on H. pylori in the stomach, because we are most aware of its link to upper GI symptoms and diagnoses like ulcers and stomach cancer. But in 2014 research was published that found H. pylori nearly everywhere in the body! The image below shows the locations H. pylori has been found, but more recent findings have highlighted its presence in the vaginal tract, kidneys and urinary tract, as well as a part of atherosclerotic plaque. The key takeaway here is that H. pylori can be found throughout the whole GI tract, not just the stomach.
Another interesting observation is that H. pylori can hide and replicate in Candida, a common yeast found throughout the GI tract and the vagina. As such, we now have evidence to support H. pylori’s link through Candida to vaginal yeast infections. Yeast provide protection for H. pylori against highly acidic and oxygen-depleted environments in the human body.
Since we know H. pylori can cause so much damage when it inhabits the stomach, let’s focus in a little here. Nobody thought bacteria could survive in the highly acidic environment of the stomach, but it is now known that H. pylori can hang out there and cause up to 80% of gastric and other GI ulcers, chronic gastritis and stomach cancer, amongst other upper GI symptoms and conditions. It manages to survive this harsh environment by burrowing into the less acidic mucosal layer that lines the stomach, and protects it from its acidic habitat.
In early phases of H. pylori colonization of the stomach, many experience low stomach acid (hypochlorhydria) and its associated symptoms. Over time, additional H. pylori strains may colonize, including those with ‘virulence factors’ that bring increased risk of symptoms and disease. More on this below. Because H. pylori can colonize its host for life, it can create chronic symptoms and long-term health complications when it becomes perpetually out of balance.
Another interesting, and relatively new learning about H. pylori is that is has a coccoid variation. This is a morphological variation which allows H. pylori to withstand stressors, it’s not culturable or easy to find on lab testing, and it can survive in extreme environmental conditions and stay in this state for twelve months! This is important to note, and in part explains why H. pylori may show on a lab 12+ months after it has previously been negative or below detectable levels.
H. pylori prevalence - how common is it?
While it is estimated that around half of the world’s population has H. pylori in the stomach, the rates vary widely by region and socio-economic status. For example, it is estimated that:
Regions with the highest rates of H. pylori are Africa (70%), South America (69%) and Western Asia (67%).
Regions with the lowest rates of H. pylori are Australia (25%), Western Europe (34%) and North America (37%).
According to the CDC, in the United States H. pylori is more prevalent among older adults, African Americans, Hispanics, Indigenous Alaskans and lower socioeconomic groups.
It is estimated that in the United States, the prevalence of H. pylori 20% for people younger than 30 years old and 50% for those older than 60.
As such, it is not ‘normal’ for those under 50 years old who aren’t from an at-risk ethnic or socio-economic group to have high levels of H. pylori in the stomach. And given the symptom profile and long term consequences of H. pylori (discussed below), eradicating it may be considered when identified on testing in symptomatic clients.
H. pylori transmission - is it contagious?
H. pylori is thought to be transmitted via saliva, vomit or fecal matter, which all makes sense now we know H. pylori can be found in the oral cavity, as well as the rest of the GI tract. The most common ways we can be exposed to H. pylori are likely:
Contaminated food or water
Poor hygiene - e.g. lack of hand washing
Kissing
Pre-chewing food given to babies.
Given the increased prevalence in certain regions, traveling to developing countries may increase your risk of H. pylori infection. However, according to the CDC, short-term travelers aren’t at significant risk of H. pylori but expats and long-stay travelers may be at higher risk.
Our body’s immune system is designed to prevent bacteria like H. pylori colonizing and overgrowing. When H. pylori is in the stomach, our major defense mechanism is stomach acid. As such, those with low levels of stomach acid may be at higher risk of H. pylori colonization. We talk a lot about stomach acid in this blog, but in short, the main contributors to low stomach acid are:
H. pylori itself, as it produces ammonia as a by-product to neutralize stomach acid
Age, as our gastric acid secretions reduce as we get older
Stress (physical and mental/emotional), which can impact the production of stomach acid
Deficiencies in vitamins or minerals essential to HCL production (e.g. zinc and vitamin B6), which may lead to low stomach acid
Proton pump inhibitors and antacids, which are specifically designed to reduce the volume and acidity of stomach acid
GI surgery (e.g. gastric bypass surgery) that can reduce the amount of stomach acid produced
Studies have also shown those with lower levels of vitamin D are more likely to have H. pylori in the stomach as an overgrowth. As with stomach acid, this is thought to be a result of vitamin D’s importance in modulating our body’s innate and adaptive immune responses.
Potential long-term consequences of H. pylori
H. pylori is most famously associated with stomach ulcers, but emerging research has also identified potential associations with a number of other conditions, including:
Gastric diseases including gastritis (inflammation of the stomach lining), bile reflux gastritis, stomach ulcers and stomach cancer
Iron deficiency anemia - H. pylori impairs iron absorption in our body
Skin disorders - found in 81% of rosacea patients who also had gastric complaints
Neurodegenerative diseases - including Alzheimer’s and Parkinson’s diseases
Autoimmune disorders - including Grave’s disease
H. pylori’s biggest side-effect appears to be its ability to produce an enzyme called urease which is hydrolyzed into ammonia to neutralize stomach acid and dampen the body’s immune response. It is this reduction in stomach acidity that allows H. pylori to continue living in what would otherwise be too harsh an environment. Because stomach acid is an important first line of defense for our immune system to kill off ingested pathogens, the risk of further infections (and subsequent conditions) also increases. If you have H. pylori showing in high amounts of testing, we tend to find other pathogens or overgrowths in the GI tract for this reason.
As part of it’s ongoing defense, H. pylori burrows into the gut lining (epithelial cells) and starts to create damage and chronic inflammation. While not everyone with H. pylori is symptomatic or develops these long-term symptoms, certain virulence factors may explain the variation from person to person. That is, not all H. pylori infections are created equal.
The importance of H. pylori virulence factors
Basically, H. pylori variants carrying specific virulence factors, or genes, can lead to more severe symptoms and health consequences. Virulence factors are molecules produced by bacteria that allow them to increase their ability to cause harm by improving colonization, suppressing the immune system and obtaining nutrition. For H. pylori these include the following genes listed in the table below, including cytotoxin-associated gene A (Cag A) and vacuolating cytotoxin A (VacA), both of which can cause tissue damage and inflammation.
This is why advanced stool testing that allows us to identify the presence of these virulence factors can help prioritize H. pylori in the eradication hierarchy, when correlated with a client’s symptoms. Virulence factors also explain why when a person is symptomatic, the theory that “half the world’s population has it so it doesn’t matter” is neither accurate nor helpful. Not all H. pylori is created equal.
H. pylori symptoms
Many clients have mild symptoms which can lead to the belief that H. pylori isn’t negatively impacting them. It becomes a hidden overgrowth that may present issues a lot later, making interventions that much more complex. But for others there may be any of the following H. pylori symptoms.
In our clinic, the most common GI signs and symptoms of H. pylori are:
Heartburn or reflux, leading to GERD - see below
Upper abdominal pain
Nausea
Burping
Bad breath (Halitosis) - particularly after eating protein
Difficulty digesting protein-heavy meals
Loss of appetite and/or feeling of fullness
Other less common GI symptoms of H. pylori include:
Bloating
Constipation
Diarrhea
Vomiting
Undigested food in the stool
Persistent dysbiosis
Gastric ulcers
Gastric Cancer
Hyperemesis gravidarum
In addition to those listed above, H. pylori can contribute to symptoms outside of the GI tract, including:
Fatigue
Acne and other skin conditions
Migraines or headaches
Anxiety and depression
Histamine symptoms like hives
Chronic dysfunction at T6 - T7 vertebral levels
Nutrient deficiency, especially iron-deficiency anema
Insomnia
Sinus and ENT issues
Acid Reflux and GERD - What’s the connection to H. pylori?
Low stomach acid is one of the causes of acid reflux and GERD. We have written a blog about this very subject which you can read about HERE. But in a nutshell, the sphincter that closes off the stomach from the esophagus after food has entered needs a certain level of acidity to seal it up properly. When stomach acid has been neutralized (lowered), the sphincter can remain open or at least not completely shut. When this happens the gastric juices can flow back up the esophagus and result in acid reflux and GERD.
So, because H. pylori neutralizes stomach acid via the production of ammonia (discussed above), it is a common root cause of acid reflux and GERD in many of our clients.
H. pylori testing: How can we find it?
A number of H. pylori testing options are available, listed below. In our experience, DNA stool testing is the most helpful tool we have available to use in clinical practice.
Breath test - a Urea breath test shows if you have H. pylori in large numbers in the stomach by analyzing a sample of your breath. While breath tests are typically accurate, safe, simple and quick to perform, they aren’t able to determine the presence of virulence factors. They are however, a particularly useful test to check whether the overgrowth has been successfully rebalanced.
Stool test - advanced DNA (PCR) stool testing is our current go-to for identifying the presence of H. pylori and virulence factors known to worsen symptoms. Older forms of stool testing didn’t have a great hit rate on identifying H. pylori, which led to many sufferers not being diagnosed correctly. A stool test can also identify other co-infections that may be contributing to GI symptoms, provide clues about digestive health function and report on virulence factors.
Blood test - These can identify a history of infection. They are not useful for checking whether the infection is current or has been successfully treated because the antibody to H. pylori (the marker of the body’s response to infection) can remain in the blood for years.
Endoscopy - H. pylori may be found at the same time as a peptic ulcer, with an invasive test called an endoscopy. H. pylori can be detected by a number of methods - including looking at samples under a microscope, using a chemical reaction or growing it in the laboratory. We have seen many endoscopy reports show no H. pylori present, but urea breath testing and DNA stool testing show H. pylori. Our current understanding is that H. pylori was not present in the part of the stomach that was biopsied, but was likely present elsewhere in the stomach, or the GI tract.
H. pylori natural treatment protocol approaches
H. pylori is thought to colonize around one third of the population in developed countries. And we know it can be a part of our normal flora, if it remains in balance. The issue lies with those who develop symptoms and lab testing demonstrates H. pylori levels that are elevated or the presence of virulence factors. For these people, establishing our goals around eradication is important. We need to work out whether we are aiming for symptom relief, eradication or reduction.
There are multiple treatment options available for H. pylori, including both antibiotics and natural antimicrobials. I recommend working with a practitioner to address H. pylori if you are symptomatic and have this bacteria in your GI tract. However, here are our suggestions and treatment approaches to consider for H. pylori.
Diet for H. pylori
Diet alone will not eradicate H. pylori, but we can introduce and remove certain foods to reduce inflammation and reliance on stomach acid during the eradication phase. The following may help reduce inflammation:
Removing inflammatory foods like processed foods, alcohol, gluten, dairy and sugar
Eating cooked rather than raw food
Smaller meal sizes
Avoiding caffeine and carbonated drinks, spicy and pickled foods
The following foods have been studied for their anti-H. pylori effects, with many clinicians including them in protocols to aid eradication:
Honey
Green tea
Flaxseed oil (contains linolenic acid, which helps address H. pylori in coccoid form)
Fish oil (omega-3 source) from supplements or oily fish like sardines, mackerel, salmon or herring
Broccoli sprouts
Garlic
Ginger
Cranberry juice
Lifestyle recommendations
Stress, whether physical or mental/emotional, reduces our production of stomach acid. As such, incorporating routines that help us reduce stress, especially around meal times can be supportive. It might sound simple, but the three most effective stress-reducing strategies we like to encourage clients to adopt include:
Replacing excessive cardio exercise with forms of movement like walking and yoga that place less stress on the body
Taking a moment before meals to slow-down, breathe and just generally be more mentally present while eating
Prioritize at least 7-8 hours of sleep per night to ensure you’re giving the body enough space to rest and repair
H. pylori natural treatment - herbals and supplements:
If you are considering a H. pylori natural treatment protocol, here are a few product options and considerations:
Herbal antimicrobials for H. pylori
For eradicating H. pylori we typically use a protocol that includes Matula Tea, Mastic Gum, Black Cumin Seed and/or Allicin (garlic extract).
Since we started using Matula Tea for H. pylori in our protocols, we have had hundreds of clients complete a protocol with rates of successful eradication of H. pylori that broadly align with the in-vitro research (commissioned by Matula Tea) on its effectiveness. Given Matula Tea for H. pylori doesn’t generally have side-effects (other than general die-off symptoms for some people), only takes 30-60 days and is in an easy to consume tea, it has been a real game-changer for our protocols. It might be about the world’s most expensive tea, but including it in our protocols has certainly improved client outcomes. You can learn more about Matula Tea and H. pylori HERE. We always use antimicrobials in combination with a number of other support products so can’t comment on the effectiveness of Matula Tea in eradicating H. pylori when taken on its own.
If we don’t use Matula Tea, we look to blended products like BioMatrix, Pylori-X or Douglas Labs, Pylori-Plex which both contain Mastic Gum. For many of our clients who have experienced symptoms that correlate with H. pylori for long periods of time, we may also add in a second antimicrobial such as Allimax Nutraceuticals, Allimed Capsules (available on our Fullscript Dispensary).
Biofilm disruptor
Like most bacterial infections, H. pylori is known to form biofilms as part of its survival and defense against eradication. As such, we commonly use a biofilm disruptor to help breakdown biofilm and assist with eradication. There are a number of products available, but the most well tolerated and effective in our experience is Biofilm Defense by Kirkman Labs or Apex Energetics, Biofilm-CLR (available on our Fullscipt Dispensary).
Probiotics for H. pylori
Probiotics have been shown to aid in eradicating H. pylori and are generally helpful in accelerating the gut healing process. Lactobacillus strains (including L. reuteri, L. fermentum, L. casei and L. brevis) have specifically been identified in scientific research for their H. pylori-fighting abilities.
More specfically, the L. reuteri DSM 17648 strain has been studied for its ability to reduce H. pylori load. This strain co-aggregates around H. pylori without negatively impacting commensal gut bacteria. You can find this strain in Microbiome Labs, PyloGuard (available on our Fullscript Dispensary).
Avoid using HCL
While some practitioners promote HCL use to combat H. pylori’s ability to reduce stomach acidity, this is not something we typically recommend. The theory is that HCL supplementation stimulates H. pylori to burrow deeper into the mucosal layer of the stomach lining to protect itself against rising stomach acid levels, further entrenching the bacteria and making it difficult to eradicate. For this reason, we err on the side of caution and avoid HCL during the eradication phase, where possible.
Liver and gallbladder support
Because H. pylori can migrate to the gallbladder and liver and cause issues with digestion of fats, using support products to help flush H. pylori from these environments is helpful for full eradication and relapse prevention. We commonly use Designs for Health, LV-GB Complex (available on our Fullscipt Dispensary).
Stomach lining support
Including additional support products such as DGL, slippery elm, marshmallow root and aloe vera can all help to soothe and heal the stomach lining both during and after H. pylori eradication. These ingredients are commonly included in the antimicrobial blends we like to use, or you can source them separately like Thorne, GI-Relief (available on our Fullscipt Dispensary). You can open the capsules of this product and make it into a soothing tea to drink between meals.
H. pylori die-off symptoms and detox support
As bacterial cells are killed, they release endotoxins into the GI tract that can provoke the immune system and cause an inflammatory response. You can learn more about die-off in THIS detailed blog post. In short, we often recommend the use of binder blends such as Biocidin Botanicals, G.I. Detox+ or Activated Charcoal to help reduce H. pylori die-off symptoms during a protocol. These act like a magnet to bind up toxins and carry them through the GI tract to be eliminated via the stool.
Vitamin D for H. pylori
Vitamin D deficiency has been shown in a number of scientific studies to negatively impact the effectiveness of antibiotic treatments. As such, and because vitamin D operates via a separate mechanism, it has also been proposed that supplementing vitamin D could increase the effectiveness of H. pylori treatment. Because those with H. pylori tend to be vitamin D deficient, it can be a good idea to supplement both during and post eradication to rebalance these levels and also assist in relapse prevention.
Access H. Pylori SUPPORT supplements FROM OUR DISPENSARY
If you are struggling with H. pylori and have been given supplement support recommendations by a health practitioner, you can likely find them and the products we often recommend to clients on our USA Fullscript Dispensary at 20% OFF RRP. You will need to set-up a Fullscript account to access our discounted pricing. Please use the Fullscript link or banner below: https://us.fullscript.com/welcome/blindemann
Antibiotics for H. pylori
Conventional antibiotics used to be the first line therapy for H. pylori. The standard triple therapy typically involves a proton pump inhibitor, amoxicillin and metronidazole. However, due to increasing antibiotic resistance to key antibiotics, and the long-term damage associated with these broad spectrum products on our gut microbiome, we prefer the H. pylori natural treatment approach discussed above. The main caveats to this would be for clients who have multiple virulence factors and a history of cancer.
Work with our practitioners to address H. pylori naturally
H. pylori in those who are symptomatic, or who have virulence factors, needs to be addressed to prevent the risk of long-term GI conditions. We encourage those who are symptomatic and think they might have H. pylori to work with a practitioner to test for and address this imbalance. If you would like to work with our team of H. pylori experts, please head to the Work With Us page to learn more about how we work online with clients to eradicate H. pylori and other root cause imbalances responsible for IBS symptoms.
Did you find this post on H. pylori Natural Treatment helpful? Want to get back to this post later? Save THIS PIN below to your Gut Healing board on Pinterest!
[This post contains affiliate links. These links do not affect the price you pay for products should you purchase after clicking through from our blog but do help support our blog and ability to create free educational content. Thank you for your support.]